Mental health counselling in Surry Hills or online
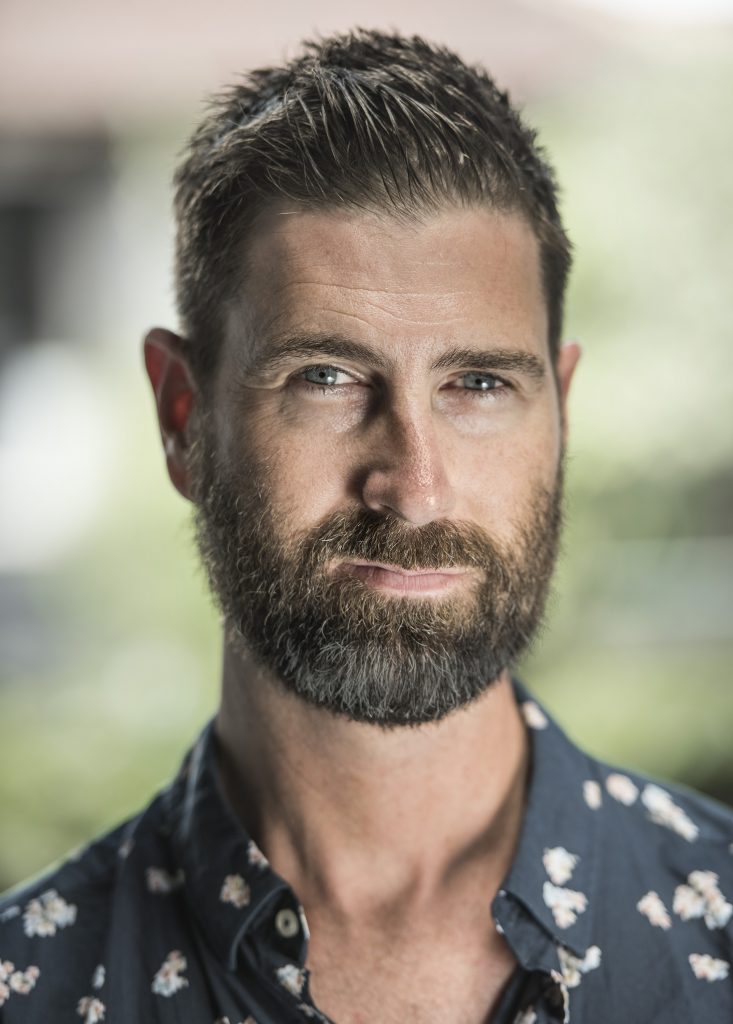
Face to face or online therapy
I’m Ash Rehn, a mental health therapist, counsellor and coach providing consultations from Surry Hills in Sydney or online.
I specialise in relationship problems, sex and sexuality related concerns, religious trauma and therapy for burnout, mid life crisis and life changes. Many people consult me about pornography use and worries about sex ‘addiction’. As a registered Medicare Provider of Focussed Psychological Strategies, I am qualified to treat anxiety, depression, adjustment and mood difficulties, psychological trauma and other mental health conditions.
Read more about my experience and qualifications.
Find answers fast at FAQ (Frequently Asked Questions).
Ready to meet? Book an appointment today.
-

Do I Have OCD? What It Means to be Obsessed or Fixated and How to Get Help
In these unsettling pandemic times, many are questioning their mental health. OCD – Obsessive Compulsive Disorder – is a condition gaining more attention. Some people find they can’t stop thinking about an event or behaviour that is starting to disrupt their life. But what does it really mean to experience OCD and how do you…
-

Retroactive Sexual Jealousy: Talk Therapy to Redefine Masculinity and Sexuality
Feeling jealous about your girlfriend or boyfriend’s, wife or husband’s sexual history can lead to obsessive thinking, suspiciousness or controlling behaviour. For some guys it’s related to sexual performance anxiety. But Retroactive Jealousy, as it is sometimes called, is usually not a sign that the relationship is under threat from another party. This sexual jealousy…
-

How to Treat ‘Sex Addiction’: The Role of the Therapist
Is sex addiction really a legitimate mental health problem or just an excuse for sleeping around? That was the question Tom Tilley used to open the Hack Live Sex Addicts programme shown on Australia’s public tv broadcaster the ABC this week. I’m sure a lot of viewers were hoping to get a handle on their…
Have any questions?